Please change the NHS treatment protocol for hypothyroidism, which is leaving so many patients sick.
Why is this important?
One in twenty adults in this country is affected by thyroid disease. Women with hypothyroidism outnumber men by ten to one.
Symptoms include anxiety and depression, cardiological problems, hair loss, lack of libido, physical pain, exhaustion, hypertension, high cholesterol and weight gain. Some GPs also tell patients that diabetes is an inevitable long term consequence. The NHS diagnosis and management of the condition is usually through one blood test which measures thyroid stimulating hormone (TSH). The lower the thyroid hormones in the pituitary gland, the more TSH the pituitary secretes. For decades now, this condition has been treated almost exclusively with Levothyroxine, a synthetic form of one thyroid hormone: T4. For most patients, T4 in the Levothyroxine converts to T3, which is then used by the body for energy.
However, for a large proportion of hypothyroidism patients, this treatment either stops working or never quite starts. Even though these people’s TSH readings might fall into the ‘normal’ range (which, depending on your GP, can be anywhere between under 5 and under 10) their symptoms soon return and worsen over time. They are then told it’s ‘all in their mind’ or due to their lifestyle, and they receive no further help to cope with an ever-decreasing quality of life. Some may, in the meantime, be prescribed anti-depressants or be diagnosed with Fibromyalgia or CFS. Others develop heart conditions, particularly atrial fibrillation, which can occur both through under and over medication: this highlights the need for a more nuanced approach to their thyroid blood tests. Most, at any rate, simply have to deal with their condition(s) on their own with very limited help from the NHS.
Much success has been achieved through some enlightened NHS endocrinologists or privately, however, using a combination of levothyroxine and liothyronine (T3) or natural desiccated thyroid, the old standard treatment before Levothyroxine.
There is a growing trend amongst patients to feel the need to take their treatment into their own hands, including more extensive blood tests to show the real extent of their thyroid’s condition and activity, and thereby more accurately gauge the effectiveness of medication. This does, however, mostly have to happen privately due to the limited guidelines of the NHS. This means that, apart from the individual expense, monitoring of the treatment and condition is not regulated and information/research is not being gathered by the extensive NHS network to improve its understanding and treatment of hypothyroidism.
We call on you to reconsider the NHS's adherence to the TSH reading as the principal guideline for diagnosing and monitoring hypothyroidism, to take patients’ symptoms more into consideration and to routinely use a full panel of FT4, FT3 and TSH blood tests for anyone still displaying symptoms of under-active thyroid, particularly when on thyroid hormone treatment.
We also call on the NHS to make the combined medication of T3 – liothyronine – with Levothyroxine much more easily available to patients whose symptoms do not sufficiently improve on T4 alone.
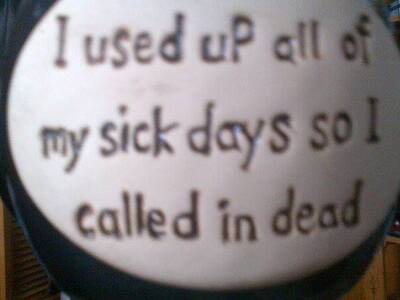
Considering the amount of work days lost and lack of quality of life for such a large number of tax payers, it is in the country’s interest that these patients should get more help. Their symptoms of exhaustion, physical pain, depression and anxiety, along with the increased tendency to develop cardiac disease and diabetes, should not be dismissed as just another malaise of middle age when there is a growing body of evidence to the contrary from people who have managed to treat themselves back to a level of health and vitality that they, and their GPs, thought they had lost for ever.
How it will be delivered